Clarion calls, COVID 19 and beyond
April 04, 2020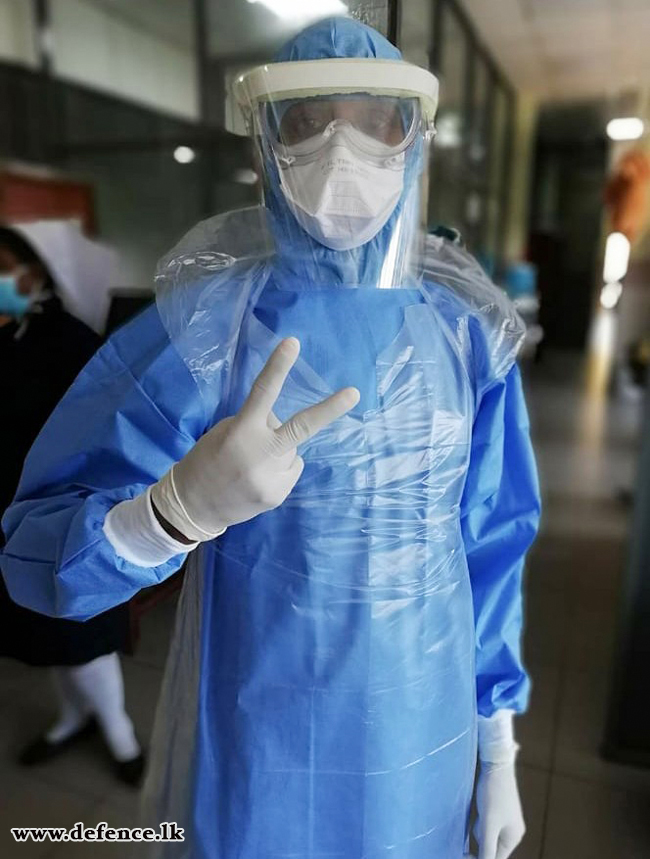 On March 28, the first death due to COVID-19 was reported in Sri Lanka. The deceased, a 60 year old was reported to have had many medical complications including diabetes and high blood pressure. The risk to elderly males from the virus is no trivia, as statistics available across the world shows over 67% of confirmed cases associated with males and over 90% deceased had some form of pre-existing medical complications.
On March 28, the first death due to COVID-19 was reported in Sri Lanka. The deceased, a 60 year old was reported to have had many medical complications including diabetes and high blood pressure. The risk to elderly males from the virus is no trivia, as statistics available across the world shows over 67% of confirmed cases associated with males and over 90% deceased had some form of pre-existing medical complications.
While, the world’s attention over the coronavirus pandemic shifted from Wuhan, its initial epi-center to Italy, March 28 became significant as United States surpassed both China and Italy on the scale of confirmed patients. This was a confirmation of the WHO prophecy, when on Tuesday (March 24), the WHO spokeswoman Margaret Harris warned that USA could become the new epi center of the pandemic.
What happened in USA in Saturday (28), had an unprecedented impact on the psyche of the entire globe, governments, health officials and people alike. While, all nations are shoring might and main to arrest the outbreak, alarms ringing in the USA’s have transcended fears and shattered illusions of a resilient America.
Rich, strong, developed and advanced USA was thought to be the readiest of all. Such expectations were no hype as according to the Global Health Security Index, the United States scored 83.5. In fact the index score for U.S is the highest. The index is a gauge of 34 indicators across 6 categories in measuring the pandemic preparedness of any given country. Sri Lanka fares a dismal index score of 33.9 but is identified to be ‘a more prepared country’ against the pandemic, out of 195 countries accounted.
Hence, all these evidence and considering the months of advance warnings that was available, America’s present situation is quite startling. Therefore, if this is the case, March 28 is indeed a clarion call to us, Sri Lankan’s that our worries are not over. We are at war. A war against a slow and stealthy microscopic organism that already has tested resilience of many well equipped health care systems. No doubt the situation is putting to test the incumbent government’s grey matter and resolve against ‘unknowns of unknowns’.
Wild, Wild West
The trillion dollar question is why has USA faltered so far in its response? Though it is difficult to draw parallels between the two health sectors, Sri Lanka has taken and executed what seem hard and difficult decisions at a time of crisis. Despite the ever soaring numbers of infected patients, the U.S administration seems to be embroiled in making lax policy responses short of aggressive measures enforcing quarantine and social distancing.
The pandemic has crossed over 50 states infecting over 120,000 individuals leaving a trail of over 2,000 deceased.
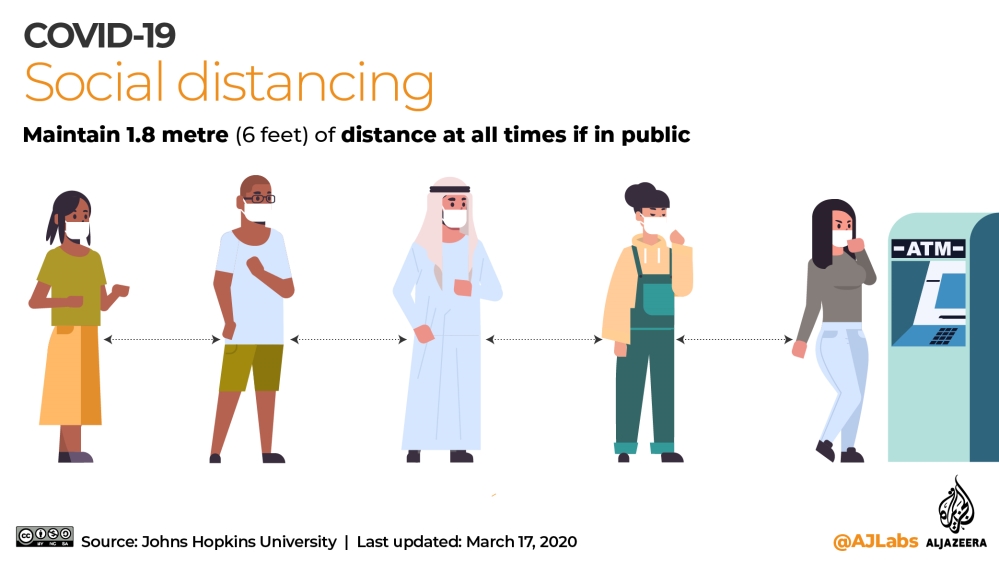
According to a study done by the University of Pennsylvania involving U.S citizens, social distancing could reduce the infection rates by 95%.
Comparing the numbers in the state of New York which is home to over 19.4 million people with Sri Lanka would at least shed a light on what our priorities should be in the coming weeks. The state of New York is as twice as large as Sri Lanka. Its population density is around 421 people per square mile which is approximately half the number in the island (884 people per square mile).
Among the confirmed cases reported, New York itself accounts to over 59,000, with a staggering number of over 900 deaths. In spite of these, the local administration has shown less interest in the idea of enforced quarantine or even to limit non-essential domestic travel.
Amidst the looming crisis its medical workers have voiced concerns over their safety in the long run. Sure a large logistic supply chain is needed to provide the gloves, masks, sanitizers, PPEs essential in protecting health care workers who are the mainstay in the pandemic response.
According to a recent estimate from the University of Pennsylvania, 960,000 Americans will still need intensive care. In addition, there are only about 180,000 ventilators in the U.S as a whole and only enough trained health and critical care staff to look after 100,000 ventilated patients. The situation in New York is direr, as the state governor Andrew M. Cuomo, revealed during a recent press conference on March 26, that New York alone required at least 40,000 ventilators to accommodate projected demands over the existing 12,000 ventilators. He feared that the state would exceed its hospital bed capacity. Meanwhile, data from the Harvard Global Health Institute estimates roughly over 1,400 ICU beds in total at the NY state’s disposal.
Where are we?
In comparison to what’s transpiring in the state of New York, we Sri Lankan’s should feel quite fortunate that the pandemic has not yet gone out of our response reach. The preemptive measures taken by the government mechanism, amalgamating its national resources into a single objective has no doubt extended much needed time to flatten the pandemic curve before it exhausts our healthcare resources. It has provided a cushion in preparing for the worst and to replenish and buffer essential stocks of PPEs, masks, ventilators, ICU treatment units etc. The measures have also foiled a trigger of nationwide panic due to fear psychosis and misinformation in crisis, avoiding a social-health catastrophe from unfolding.
In military terms, the government has activated all lines of operations at its disposal. Though not drastic and hasty the measured approach undertaken is the highlight of Sri Lanka’s response. So far the state apparatus is seen taking pragmatic decisions in response to the evolving global situation and signals emitting domestically across all sectors.

Yet are we safe, is the billion dollar question. A projection into the domestic health care system should incentivize policy makers and public at strict compliance towards social distancing and standardized sanitary and hygienic practices. It is learnt that the total ICU bed capacity in Sri Lanka is just over 510. The ratio of availability of ICU beds to New Yorkers is around 1: 13,900; whereas the domestic ratio is around 1: 41,000. The deficit is apparent which is over three folds minus than the availability to New Yorkers. Yet, this is no surprise given the stages of development of the demographics. These numbers may provide a baseline for our health authorities in preparing and forecasting in where we want to be in the event of a peak in the infected numbers.
As the article is been structured, the United States top infectious disease expert, Dr. Anthony Fauci is on record speculating over 100,000 deaths in the country over the coming weeks. Already the count has spiked over 2,500.
Unknown of unknowns
What’s worrying is the intensity of the spread of the virus. According to available evidences, the SARS-CoV2, the pathogen which causes COVID-19 disease is gaining momentum. The first 100,000 patients were reported in 67 days; second 100,000 in 11 days; third 100,000 in 4 days. Already the global figures have exceeded 700,000 infections. Hence, these numbers suggest that the virus infections must be multiplying at a rate of hours currently.
The transmission potential of a disease is measured through its R0 or the ‘Reproductive number’. The Imperial College Group estimated the R0 for the SARS-CoV2 to be in a scale of 1.5 to 3.5. For the 2014 Ebola virus the R0 figure was between 1.51 to 2.53. The R0 number for Measles is between 12 to 18 making it highly infectious. Hence, health authorities will be concerned in pushing the R0 figure for SARS-CoV 2 below 1.
Necessary Evils
So what should be our response priorities in flattening the pandemic curve? There are a few international case studies where we could draw inferences: South Korea, Singapore and Hong Kong. Though initially engulfed in a brutal battle against the pandemic, they developed tests at identifying infected people. Subsequently, the infected patients were isolated, and further those who had recently associated were traced and made to undergo strict social distancing and self-quarantine procedures. Given Singapore’s healthcare system it is easy to track and trace potential or suspected individuals. Similarly, the Sri Lankan health sector should integrate technology to its armour enhancing its pandemic response capacity; force multipliers.
In contrast to the above experiences, this is what the USA did not do. Instead of enforcing strict restrictions over travel domestically and internationally, the United States issued a ‘strong travel advisory’.
Right now Sri Lanka might be in the eye of the storm and evasive measures are needed to get away from its turbulent path. In spite of ad-hoc campaigns and donations to amass masks, gloves and PPEs a coordinated centralized effort is likely to increase equitable and efficiently allocation of the donations to hospitals/quarantine facilities ensuring the health sector stays healthy. With the possibility of depleting stocks due to rising global demands, the local supply chains needs to be revamped in manufacturing and distributing medical equipment and PPEs. Failure to do so would lead to an inevitable collapse of the system and worsening the situation.
Further, the medical tests required to confirm the disease need to be made accessible to the public while also ensuring safety of those who are administering the tests.
Finally, a strong and consistent message needs to be communicated to the public incentivizing social-distancing. Possible social nudges are to be prescribed as appropriate as a necessary evil for strict compliance. According to a study done by the University of Pennsylvania involving U.S citizens, social distancing could reduce the infection rates by 95%.