Fauci: No scientific evidence the coronavirus was made in a Chinese lab
May 07, 2020
Anthony Fauci has been the director of the U.S. National Institute of Allergy and Infectious Diseases for almost 40 years, where he has tackled dozens of outbreaks, including HIV/AIDS. To him, the coronavirus is "extraordinary."
Photograph by Mark Thiessen, National Geographic
Anthony “Tony” Fauci has become the scientific face of America’s COVID-19 response, and he says the best evidence shows the virus behind the pandemic was not made in a lab in China.
Fauci, the director of the U.S. National Institute of Allergy and Infectious Diseases, shot down the discussion that has been raging among politicians and pundits, calling it “a circular argument” in a conversation Monday with National Geographic.
“If you look at the evolution of the virus in bats and what's out there now, [the scientific evidence] is very, very strongly leaning toward this could not have been artificially or deliberately manipulated … Everything about the stepwise evolution over time strongly indicates that [this virus] evolved in nature and then jumped species,” Fauci says. Based on the scientific evidence, he also doesn’t entertain an alternate theory—that someone found the coronavirus in the wild, brought it to a lab, and then it accidentally escaped.

Dr. Anthony Fauci and Dr. Deborah Birx, White House coronavirus response coordinator, listen as President Donald Trump speaks about the coronavirus in the James Brady Press Briefing Room of the White House, Thursday, April 9, 2020, in Washington, D.C.
Photograph by Andrew Harnik, AP Photo
Fauci is most concerned that the United States will be put to the test this fall and winter by a second wave of COVID-19 if the country does not blunt the infection rate by the summer.
“Shame on us if we don't have enough tests by the time this so-called return might occur in the fall and winter,” he says, advising that the U.S. needs to make sure we not only have an adequate supply of tests available before a second wave hits, but also a system for getting those tests to the people who most need them.
“I don't think there's a chance that this virus is just going to disappear,” he says. “It's going to be around, and if given the opportunity, it will resurge.” As such, Fauci says the U.S. should also focus this summer on properly reinforcing the nation’s health care system, ensuring the availability of hospital beds, ventilators, and personal protective equipment for health care workers.
He also stressed the importance of continuing to social distance everywhere until the case counts start to fall in cities and states. The U.S. witnessed about 20,000 to 30,000 new cases every day in the month of April, suggesting the country is stuck in its peak.
Still, he remains optimistic that a vaccine will be ready within an historically short time frame, citing one promising candidate that he thinks may move into advanced clinical trials by the early summer. Fauci has said that he thinks a final vaccine could be available for general use as early as January, which would break records for the speed at which previous vaccines were developed.
One reason for his confidence is the “impressive” results being seen now in animals tested with a vaccine candidate made by Cambridge, Massachusetts-based Moderna Therapeutics, which brought it into human trials in a record 42 days. The candidate is what is known as an mRNA vaccine—a drug that uses snippets of a virus’s genetic material—rather than the dead or weakened virus itself—to build the proteins that trigger the body’s protective immune response.
To date, no type of mRNA vaccine has been licensed for use in humans, but Fauci believes there is great promise for this technology targeting the coronavirus, based in part on his experience developing treatments for HIV/AIDS in the 1980s and ‘90s.
“For some reason that we're still struggling with, the body does not make an adequate immune response to HIV,” he says. To fight off that virus, a vaccine has to work better than the body’s own natural response. By contrast, “it's obvious that many people make a very adequate immune response” to the SARS-CoV-2 virus, and the animal trials so far show that modest doses of the mRNA vaccine for coronavirus have also generated a strong immune response.
He adds that NIAID is still developing and supporting multiple vaccine efforts, in case those that go into trials soonest don’t ultimately prove safe and effective. “You want a lot of shots on goal. We want four or five candidates that we put out there all within a reasonable time,” he says.
Fauci told National Geographic he’s concerned about states rushing to reopen before their infection rates fall. He also shared how he manages the barrage of new scientific information being released about COVID-19, and how his family and faith keep him going despite his increasingly hectic schedule.
(The following interview has been edited for length and clarity.)
Fauci on the vaccine
You’ve been the NIAID director since 1984, witnessing dozens of disease outbreaks. One of the first was the HIV/AIDS epidemic. How does that experience compare with COVID-19?
One of the important advantages is what we call targeted drug development. Viruses cause disease by binding to receptors on cells in your body, be they in your upper airway or in your lung, in the case of COVID-19. They then replicate at a rapid rate that triggers a variety of pathogenic processes. Targeting drugs to interfere at one or more vulnerable sites within this replication cycle is something that we learned with HIV.
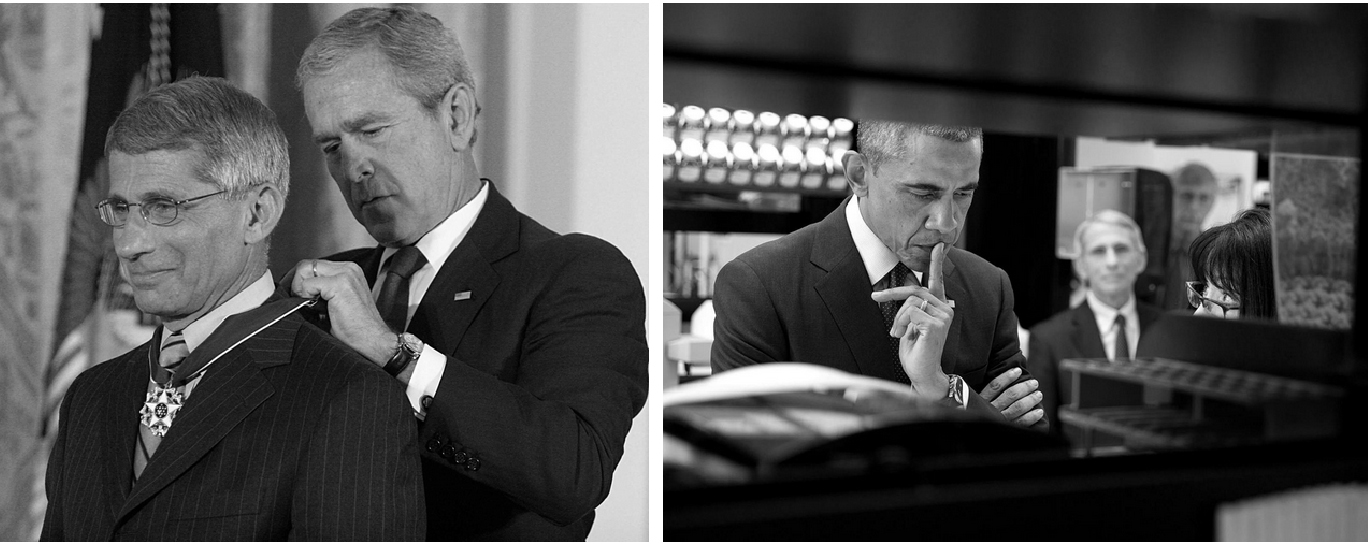
Left:
U.S. President George W. Bush presents the Presidential Medal of Freedom on June 19, 2008 to Anthony Fauci, director of the National Institute of Allergy and Infections Diseases, in Bethesda, Maryland during ceremonies at the White House. The Presidential Medal of Freedom, the nation's highest civilian award, recognizes exceptional meritorious service.
Right:
U.S. President Barack Obama listens to Dr. Nancy Sullivan, chief of the biodefense research section at the National Institute of Allergy and Infectious Diseases, explain the investigational Ebola vaccine candidate being tested on humans during a lab tour at the Vaccine Research Center at the National Institutes of Health in Bethesda, Maryland on December 2, 2014. Dr. Anthony Fauci and Dr. Francis Collins, NIH director, watch in the background.
Photograph by Karen Bleier, AFP via Getty Images (Left) and Photograph by White House Photo / Alamy Stock Photo (Right)
SARS-CoV-2 [the virus that causes COVID-19] has the same sort of vulnerable points. We need to identify them and develop drugs, either alone or in combination, to block the replication.
Are there also lessons from HIV/AIDS that relate to developing a COVID-19 vaccine?
Vaccines are a bit different. We have a better chance of quickly getting, relatively speaking, a vaccine for the novel coronavirus than we did for HIV, because for some reason that’s still unknown the body does not make an adequate immune response to HIV.
We don't necessarily have that challenge with this coronavirus because it's obvious that many people make a very adequate immune response. They clear the virus, and they do well. As we know from the natural history of this disease, the majority of people actually either get well without any symptoms—they're called asymptomatic—or they have minimal symptoms, where they get a fever, some aches, and then they recover.
The fact that the majority of people can actually clear the virus is a very good sign for the feasibility of developing a vaccine.
The two most widely discussed vaccine candidates are an mRNA vaccine from Moderna, which reached human trials in a record 42 days, and Oxford University’s candidate, based on what’s known as a nonreplicating viral vector. Yet no vaccine based on these two technologies has ever been licensed for human use. What makes these two vaccines seem so promising, especially on this expedited timeline?
These vaccines are inducing, at least in animal models, really rather substantial immune responses, particularly the mRNA vaccine. When we look at the immune response that you can induce with a modest dose—one that's feasible to be translated into humans—and the amount of time it takes to get to that level of immunity, it is really quite impressive. It is also really easy to scale up with these two, in the sense of making a lot of doses pretty quickly. So you're right, they have not been approved, as many of the other vaccine platforms have, but the promise is great.
We at NIAID are either developing or supporting the development of multiple candidates. You want a lot of shots on goal. We want four or five candidates that we put out there all within a reasonable time—maybe June, July, or August—to get them into an advanced trial. The mRNA one is already well into phase one of clinical trials, and we're getting ready to go into phase two and three sometime in the early summer.
Fauci on reopening and masks
As states move to reopen businesses and warmer weather lures people outside, how concerned are you about a fresh spike in infections in the U.S.?
Take a look at the guidelines for Opening Up America Again. There are very well delineated checkpoints. There's a gateway where infections must go down for 14 days before you can enter into phase one for reopening. If you fulfill the requirements of phase one, you move to phase two. If you do it there, you go to phase three.
So when you see somebody in an environment in which the infections are not going down, and then you see 30 to 40 people on a beach with no mask … well that's very nice to have fun in the sun, but you're really putting yourself and everyone at risk for creating an even bigger spike in infections.
Do you fear a second wave?
What’s impressed me the most—but clearly in a disturbing way—is the extraordinary efficiency of how the virus spreads. It spreads so much more efficiently than influenza does. You see situations where people at home try and physically separate; they have no contact except they've touched the plate or a doorknob, and they wind up getting infected.
The clusters in families, the outbreaks on the Teddy Roosevelt aircraft carrier, the enormous spread on the Diamond Princess cruise ship in Yokohama harbor—it’s a very, very transmissible virus.

Anthony Fauci hugs Nina Pham, the nurse who was infected with Ebola from treating patient Thomas Eric Duncan in Dallas, as Pham's mother Diana (sixth from left) and sister Cathy (fourth from left), and Director of the National Institutes of Health Francis Collins (left) look on at the end of a news briefing at NIH on October 24, 2014 in Bethesda, Maryland. Pham was declared free of the virus.
Photograph by Alex Wong, Getty Images
We're going to be put to the test as we move toward the fall and winter of this year. If we do it correctly, then we could be able to blunt and diminish the daily rate of infections in this country as we get into the summer. I can't guarantee it, but if we do things right, that likely will happen.
But I don't think there's a chance that this virus is just going to disappear. It's going to be around, and if given the opportunity, it will resurge. We now will have a few months—May June, July, August—to prepare, by making sure our health system is adequately supplied with ventilators, ICU beds, personal protective equipment, etcetera. We need to not only have tests, but to make sure the people who need tests can get tested.
So that by the time we get to September, we don't have the dialogue continually fixating on do you have enough tests? Shame on us if we don't have enough tests by the time this so-called return might occur in the fall and winter.
What’s your position on the general public wearing face masks?
I'm glad you asked, because it has evolved over the weeks and months. When there was first discussion, it was at a time when face masks—either surgical masks or N95 respirators—were at high scarcity.
Let's assume that we now have enough masks or that you could easily make a cloth covering, as was suggested appropriately by the Centers for Disease Control and Prevention. I think those are reasonable assumptions. We know that the masks are better in the health-care setting to prevent someone who's infected from coughing and sneezing and infecting people in the environment. When you look at what the mask does for the general population, the data are not 100 percent: It doesn't 100 percent protect you from infecting somebody else, and it certainly doesn't 100 percent prevent somebody else from infecting you.
But if you wear a mask, you are getting some protection for yourself, and if you happen to be infected and don't know it, you're to some extent preventing transmission to someone else. Given that, it just makes sense that first of all, the best way to prevent spread is to maintain the physical distance of six feet.
So, if you're in a situation where you're in contact with no one, then you don't have to be walking around with a mask all day, that's for sure. But if you are in a situation where you are going to be within the realm of six feet—the grocery store or even walking out on the street—then wear it.
Fauci on the information deluge and the “virus made in Chinese lab” claim.
How do you keep up with the barrage of information and filter down to the most important science?
It's like drinking from a fire hydrant. It really is. Fortunately for me, I have a staff of three to four really good people who sift through the papers and when something looks unreasonable or “pie in the sky,” they don't bother me with that. Then when all of these studies come across my desk, I read the title and the abstract. If it looks feasible, I'll put it aside and try and read it. When it's something that they think I should read, they make sure I read it.
Even with that screening process, it's still very difficult to consume everything that's out there, particularly with this relatively recent trend with these non-peer-reviewed, pre-publications [that have not gone through traditional vetting to appear in major journals].
So, what's your advice to the public at-large for sifting through the headlines and making sense of it all?
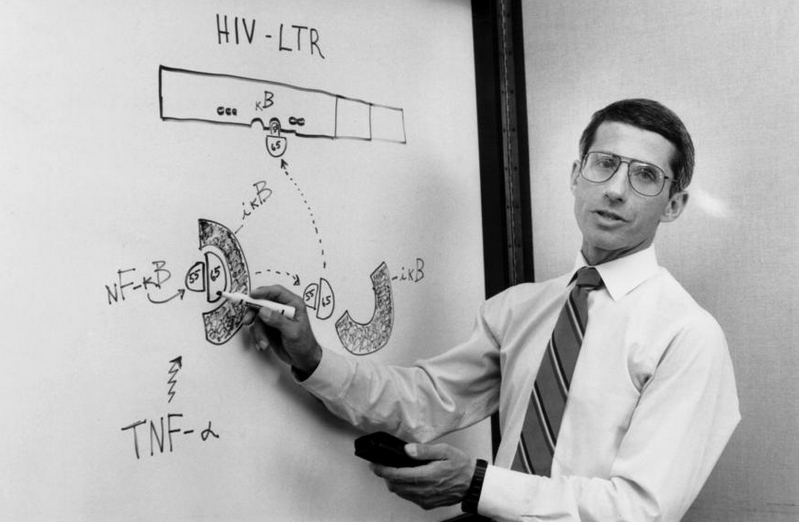
Dr. Anthony Fauci speaks with members of his laboratory during a meeting Aug. 31, 1990, where he describes a natural growth factor that is necessary for the AIDS virus to multiply.
Photograph by George Tames, The New York Times via Redux
Anybody can claim to be an expert even when they have no idea what they're talking about—and it's very difficult for the general public to distinguish. So, make sure the study is coming from a reputable organization that generally gives you the truth—though even with some reputable organizations, you occasionally get an outlier who's out there talking nonsense. If something is published in places like New England Journal of Medicine, Science, Nature, Cell, or JAMA—you know, generally that is quite well peer reviewed because the editors and the editorial staff of those journals really take things very seriously.
One topic in the news lately has been the origins of SAR-CoV-2. Do you believe or is there evidence that the virus was made in the lab in China or accidentally released from a lab in China?
If you look at the evolution of the virus in bats, and what's out there now is very, very strongly leaning toward this [virus] could not have been artificially or deliberately manipulated—the way the mutations have naturally evolved. A number of very qualified evolutionary biologists have said that everything about the stepwise evolution over time strongly indicates that it evolved in nature and then jumped species.
Sure, but what if scientists found the virus outside the lab, brought it back, and then it escaped?
But that means it was in the wild to begin with. That's why I don't get what they're talking about [and] why I don't spend a lot of time going in on this circular argument.
Fauci’s life right now
What’s your typical day like?
I get up around five o'clock in the morning, and I usually wind up running downstairs, getting a quick breakfast, and looking at a thousand emails—literally a thousand.
I then head to the NIH [National Institutes of Health] for my day job—trying to develop a vaccine and drugs and running a $6 billion institution. I stay there until around one o'clock, and then I go down to the White House for multiple meetings. First, I meet with the doctor group—myself, coronavirus response coordinator Debbie Birx, director Bob Redfield from the CDC, commissioner Steve Hahn from FDA, and others. We then go into the task force meeting run by Vice President [Mike Pence], which usually lasts about an hour and a half. We summarize this pre-brief with the vice president and then go brief President [Donald Trump] for the press conference.
Then, the work starts … I head home or back to the NIH and work until the wee hours of the morning. The whole day is punctuated by everybody needing to talk to you: every governor in the states, every congressional leader, every leader in the White House. It's constant conference calls. It's an almost impossible situation—and that's seven days a week.
Then you superimpose upon that all the press you do—the TV or the radio or the interviews. It's kind of a surrealistic state. I have to wake up in the morning and literally, without being facetious, ask my wife, what day is it?
Wow, how do you unwind?
I power walk with my wife, usually at night or on the weekends. It's dark, but we still do it anyway.
Has it ever been too taxing?
A couple of months ago, I was foolish and just thought I could get away with almost no sleep. I mean, like three hours a night. I did that for a few weeks, and it almost killed me. It really wore me down badly. Thank goodness I have a very intelligent and clinically skilled wife who turned things around and said, You got to remember to eat, and you've got to remember to sleep. The day is still impossible, but I don't think I'm going to drop dead from it. I hope not.
You went to a Jesuit high school, where you learned the importance of doing good for the public. How has that experience informed your professional life?
My whole life was almost served to me on the basis that my mother and father were very much oriented toward service. They were never really interested in money or material things. That's just the way they were, both of them. So I never knew there was anything like going out there and making a lot of money, and that was really cemented when I went both to a Jesuit high school and a Jesuit college, where the entire theme was service for others.
I almost never had any other inkling of doing anything except something that would have a public service component to it. I'm very much of a people person, but I'm also scientifically inclined. My entire training is steeped in the humanities, and when you combine that with an aptitude for science, you wind up being a physician.
Courtesy: National Geography